The global development community has worked hard to develop effective HIV prevention and treatment strategies as well as strategies to help people living with HIV (PLHIV) adhere to HIV treatment and improve their quality of life. These strategies have helped decrease the number of new HIV cases as well as AIDS-related deaths.
FANTA is contributing to these global efforts by using social and behavior change (SBC) to help people living with HIV (PLHIV) maintain good nutrition and adhere to their treatments. In a recent interview, Mary Packard, FANTA’s Technical Advisor on Social and Behavior Change Communication, described how SBC is being applied to help PLHIV.
How is SBC being used in nutrition interventions for specific groups, such as PLHIV? Also, how does it complement and/or differ from other nutrition interventions for PLHIV?
SBC is being used at different levels to support nutrition for vulnerable groups like pregnant and lactating women, infants and young children, and people living with HIV and other infectious diseases. At the national level, FANTA has supported ministries of health in Côte d’Ivoire and Mozambique to develop social and behavior change and communication strategies for nutrition. We work with local stakeholders to identify target audiences, behavior change and communication objectives, key messages, and communication channels, and we provide guidance on how to design SBC interventions that tailor activities and materials to the needs of specific groups.
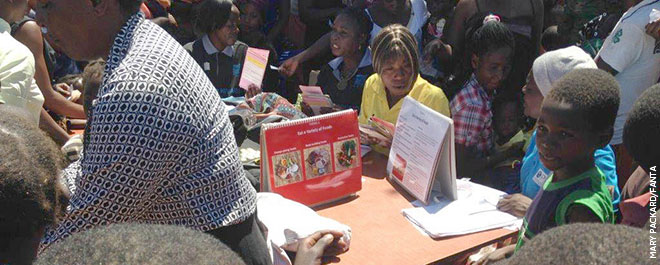
At district and community levels, FANTA provides capacity strengthening on SBC approaches for the nutrition assessment, counseling, and support (NACS) platform, which provides nutrition services for PLHIV in many countries. We train health workers in nutritional counseling and develop communication materials for use in counseling, group education, and community outreach.
One of the hallmarks of SBC is that rather than simply applying global scientific data, it uses data on behavioral drivers grounded in the local context. We collect information on such things as local cultural concepts related to health and nutrition, and barriers to the use of community resources. This information enables us to create messages about the importance of nutrition and antiretroviral therapy (ART) adherence that are truly “actionable” for PLHIV, and to facilitate the delivery of them in ways that resonate with targeted groups.
What makes SBC effective? Also, is there evidence showing that it is as effective or even more effective than other nutrition interventions for PLHIV?
There is a growing evidence base showing that SBC interventions are indeed effective, largely because their grounding in local, contextualized data enables service providers to meet people where they are and respond to the barriers and motivators to change that affect them. Also, SBC complements the more top-down interventions found in clinical services with interventions that draw on feedback and data from the clients themselves. Clients are reached through interpersonal communication, one-on-one interaction with providers at the clinic, printed materials in the clinic and the community, mass media, and volunteers who make home visits and conduct group activities in the community. Social change comes when people are touched in multiple ways with key messages; when they are armed with information, skills, and confidence arising from experience with quality SBC activities; and when they see people around them reinforcing new norms.
Can SBC also be applied at the community level? And does community SBC differ from individual SBC?
Yes—there are three mutually reinforcing elements in SBC:
- Advocacy to obtain resources and political/social commitment to particular actions and goals
- Social mobilization to enlist broad participation, build coalitions and ownership, and mobilize communities around new practices and norms
- Behavior change communication to educate and stimulate changes in attitudes and practices among specific target groups
Sometimes, those who most need nutrition services are the least likely to go to clinics. So, community outreach is essential to engage and retain them in care and to reinforce the SBC messages delivered in facility settings. Group activities such as talks given at self-help group meetings for PLHIV, cooking demonstrations for mothers, and individualized support given at events like community growth monitoring, are all ways that community SBC complements individual counseling. FANTA supports SBC activities to improve linkages between clinics and communities as well as patient outcomes.
Can community-level SBC help PLHIV in ways that other interventions, even individual SBC, cannot? How so?
Individual counseling at the health facility can go only so far in changing behavior, because behaviors happen in household and community contexts where a client is under the influence of family, friends, community leaders, and broader social forces. These influences can dominate and render ineffective the advice given by health care providers. For example, a new mother may be encouraged to practice exclusive breastfeeding by a nurse and through posters at the clinic, but her mother-in-law may not support that practice back home. SBC at the community level is crucial because it reaches not just the new mother, but also her mother-in-law, her husband/partner, and community leaders.
Good nutrition and strict adherence to ART are both crucial for successful HIV treatment. While it is essential to provide individual adherence and dietary counseling in the clinic, PLHIV who participate in community-based activities like peer support group meetings benefit in ways they would not otherwise. For example, community-based workers use SBC to facilitate sharing of strategies among peers for navigating the challenges of drug adherence, managing ART side effects through diet, and tapping into community groups for psychosocial and economic support.
What are some of the main barriers to behavior change facing communities in relation to improving people's nutrition and health? And how can community-level SBC help address these?
Some of the barriers to good nutrition relate to food insecurity and poverty. These large structural forces may be difficult for one project to resolve. But FANTA works with local health service providers to use SBC to do more than educate people about the importance of a diverse diet. We also assist with linking people to community-based resources for economic strengthening, food and welfare support, and help engage people in SBC activities that have proven effective to expand household food options at little cost, such as home gardening and food preservation.
Other barriers to good nutrition relate to food preferences and insufficient knowledge about the benefits of nutrition, which can best be addressed socially through education embedded in fun group activities such as cooking demonstrations and by mobilizing “positive deviants” or role models in the community who can testify to the benefits of behavior change.
Beyond nutrition, PLHIV face the extra burden of adhering to their drug treatment. FANTA has used community assessments, individual interviews, and group activities to gain community members’ perspectives on the barriers to ART adherence as well as diet diversity. Two of the most cited barriers to drug adherence identified in the context of FANTA’s Zambia program in Kitwe, Copperbelt Province are:
- Lack of food (some medications are intolerable on an empty stomach), which is addressed through some of the above mentioned strategies.
- Stigma-induced non-disclosure. Many ART patients don’t take their medicine because they are trying to keep their HIV status hidden from household members. For this barrier, we work with community-based support groups who share strategies for disclosure and tips for managing medicine discretely, train community volunteers in the basics of ART and adherence counseling, and provide them with information about community resources and referral capacity.
How is FANTA currently strengthening community level SBC to help people living with HIV (e.g., Zambia)?
FANTA’s flagship community SBC program is underway in Zambia, where we are developing SBC approaches focused on training and supporting community NACS volunteers to improve nutrition and ART-related practices among PLHIV in target communities. The first step was to conduct a landscape analysis and community assessment to identify local needs and resources, along with factors that support and inhibit the key recommended practices (e.g., eating a diet of adequate quantity and quality, HIV testing, and adherence to care and treatment). From this, we developed an SBC strategy to build linkages between communities and facilities. We hired a community engagement officer who is dedicated to strengthening community-level SBC. We trained the community NACS volunteers in NACS, followed by a more intensive, skills-based training in interpersonal communication to develop their capacity to identify and address behavioral determinants through individual counseling and group work.
The community engagement officer provides direct support to community volunteers, and FANTA supports sustainability by building the capacity of Ministry of Health staff to supervise the volunteers. This requires buy-in from local partners, such as government officials and community-based organizations, which we develop through a sensitization process to forge a good understanding of SBC principles and the value of investing in community activities.
Find out how other organizations are marking World AIDS Day: